hemalbhagat@hotmail.com
Get a Consultation
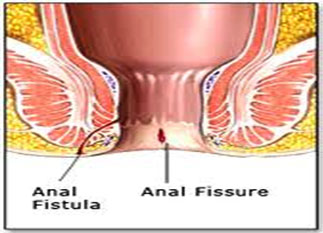
An anal fissure is a break or tear in the skin of the anal canal. Anal fissures may be noticed by bright red anal bleeding on the toilet paper, sometimes in the toilet. If acute they may cause pain after passing stools but with chronic fissures pain intensity is often less.
Most anal fissures are caused by stretching of the anal skin beyond its capability.
In adults, fissures may be caused by
Other common causes of anal fissures include:
For adults, the following may help prevent anal fissures:
Medication
Non-surgical treatments are recommended initially for acute and chronic anal fissures.These include topical nitroglycerin or calcium channel blockers, or injection of botulinum toxin into the anal sphincter.
Other measures include:
Surgical
The procedure is generally performed as a day surgery after the patient is given necessary anesthesia. The pain from the sphincterotomy is usually mild and is often less than the pain of the fissure itself. Patients often return to normal activity within one week.
LIS does, however, have a number of potential side effects including problems with incision site healing and incontinence to flatus and faeces
Following lateral internal anal sphincterotomy constipation can be particularly unpleasant and painful so it is important to keep the bowel motions soft and regular.
Drink at least six to eight glasses of water a day. A high-fibre diet is recommended including plenty of cereal fibre, fresh fruit and vegetables. You may require a stool bulking agents.
Hygiene - it is important to keep the area clean and dry. Avoid using dry toilet paper, instead use a warm flannel or moist soft tissues. Saline baths (a cup of salt per bath) several times daily especially after bowel movements are good for hygiene and are very soothing.
These are very uncommon as the operation is simple and safe. Rarely, there may be postoperative bleeding. In approximately five percent of patients the healing of the wound may be delayed.
The small incision in the internal anal sphincter (sphincterotomy) may result in a slight imperfection in the control of "wind" in the rectum i.e. passage of flatus. This is usually a temporary problem. Incontinence of faeces (loss of control of bowel movements) is an extremely rare complication.
Approximately 1-6% of patients have a recurrence of their anal fissure after sphincterotomy. The recurrence rate is higher after a sphincter stretch